Contents :
The Male Genital System
The Testis
Spermatogenesis
Genital Ducts
Genital Accessory Glands
The Penis
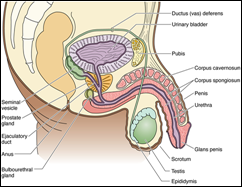
The Male Genital System
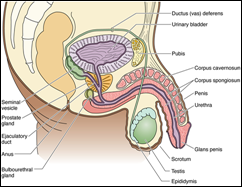
The male reproductive (genital) system consists of the
two testes suspended in the scrotum, a system of
intratesticular and
extratesticular genital ducts,
associated glands, and the
male copulatory organ, the penis. The testes are responsible for the formation of the male gametes, known as spermatozoa, as well as for the synthesis, storage, and release of the male sex hormone, testosterone.
The glands associated with the male reproductive tract are the paired seminal vesicles, the single prostate gland, and the two bulbourethral glands (of Cowper). These glands form the non-cellular portion of semen (spermatozoa suspended in the secretions of the accessory glands), which not only nourishes the spermatozoa but also provides a fluid vehicle for their delivery into the female reproductive tract.
The penis has a dual function: It delivers semen to the female reproductive tract during copulation and serves as the conduit of urine from the urinary bladder to outside the body.
TESTIS

Each testis is surrounded by a capsule known as the
tunica albuginea. Immediately deep to this layer is a highly vascularized loose connective tissue,
the tunica vasculosa. The posterior aspect of the tunica albuginea is somewhat thickened, forming the
mediastinum testis, from which connective tissue septa radiate to subdivide each testis into approximately 250 compartments known as the
lobuli testis
Each lobule has one to four blindly ending seminiferous tubules and small conglomerations of endocrine cells, the interstitial cells (of Leydig) which synthesize testosterone.
Spermatozoa, produced by the seminiferous epithelium of the seminiferous tubules, enter short straight ducts, tubuli recti, that connect the open end of each seminiferous tubule to the rete testis, a system of labyrinthine spaces housed within the mediastinum testis. The spermatozoa leave the rete testis through 10 to 20 short tubules, the ductuli efferentes, which eventually fuse with the epididymis.
The vascular supply of each testis is derived from the testicular artery, which descends with the testis into the scrotum accompanying the ductus deferens (vas deferens).
The capillary beds of the testes are collected into several veins, the pampiniform plexus of veins, which are wrapped around the testicular artery.
Blood in the pampiniform plexus of veins is cooler than that in the testicular artery, reduces the temperature of the arterial blood, thus forming a countercurrent heat exchange system, keeping the temperature of the testes a few degrees lower (35˚ C), than that of the remainder of the body. At this cooler temperature spermatozoa develop normally; at body temperature, spermatozoa that develop are sterile.
THE SEMINIFEROUS TUBULE

The wall of the seminiferous tubule is composed of a slender connective tissue layer, the tunica
propria, and a
thick seminiferous epithelium, separated from each other by a well-developed basal lamina.
The seminiferous epithelium is several cell layers thick and is composed of two types of cells: Sertoli cells and spermatogenic cells. The latter cells are in various stages of maturation.
The lateral cell membranes of adjacent Sertoli cells form occluding junctions with each other, thus subdividing the lumen of the seminiferous tubule into basal and adluminal compartments. Thus, the zonulae occludentes of these cells establish a blood-testis barrier that isolates the adluminal compartment from connective tissue influences, thereby protecting the developing gametes from the immune system..
Sertoli cells function in: supporting the developing spermatogenic cells; establishing the blood-testis barrier; phagocytosis of cytoplas shed by developing spermatogenic cells; manufacturing the following substances: androgen binding protein (ABP), antimullerian hormone, inhibin, testicular transferrin, and a fructose-rich medium.
SPERMATOGENESIS
Most of the cells composing the thick seminiferous epithelium are spermatogenic cells in various stages of maturation. Some of these cells, spermatogonia, are located in the basal compartment, whereas most of the developing cells—primary spermatocytes, secondary spermatocytes, spermatids, and spermatozoa—occupy the adluminal compartment.
Spermatogonia are diploid cells that undergo mitotic division to form more spermatogonia as well as primary spermatocytes, which migrate from the basal into the adluminal compartment.
Primary spermatocytes enter the first meiotic division to form secondary spermatocytes, which undergo the second meiotic division to form haploid cells known as spermatids.
Spermatids are transformed into spermatozoa by shedding of much of their cytoplasm, rearrangement of their organelles, and formation of flagella.
The maturation process is divided into three phases:
–Spermatocytogenesis: spermatogonia differentiate into primary spermatocytes
–Meiosis: reduction division whereby diploid primary spermatocytes reduce their chromosome complement, forming haploid spermatids
–Spermiogenesis: transformation of spermatids into spermatozoa (sperm)
SPERMATOZOON

Spermatids discard much of their cytoplasm and form a flagellum to become transformed into spermatozoa, a process known as spermiogenesis.
The spermatozoa (sperm) are long cells (~65 μm), composed of a head, housing the nucleus, and a tail, which accounts for most of its length
The tail of the spermatozoon is subdivided into four regions: neck, middle piece, principal piece, and end piece. The plasmalemma of the head is continuous with the tail’s plasma membrane.
The neck (~5 μm long) connects the head to the remainder of the tail. It is composed of the cylindrical arrangement of the nine columns of the connecting piece that encircles the two centrioles, one of which is usually fragmented. The posterior aspects of the columnar densities are continuous with the nine outer dense fibers.
The middle piece (~5 μm long) is located between the neck and the principal piece. It is characterized by the presence of the mitochondrial sheath, which encircles the outer dense fibers and the centralmost axoneme. The middle piece stops at the annulus. Two of the nine outer dense fibers terminate at the annulus; the remaining seven continue into the principal piece.
The principal piece (~45 μm long) is the longest segment of the tail and extends from the annulus to the end piece. The axoneme of the principal piece is continuous with that of the middle piece. Surrounding the axoneme are the seven outer dense fibers that are continuous with those of the middle piece and are surrounded, in turn, by the fibrous sheath.
The end piece (~5 μm long) is composed of the central axoneme surrounded by plasmalemma. The axoneme is disorganized in the last 0.5 to 1.0 μm.
GENITAL DUCTS
Intratesticular Genital Ducts

The intratesticular genital ducts are the
tubuli recti (straight tubules), the
rete testis, and the
ductuli efferentes. These ducts carry spermatozoa and liquid from the seminiferous tubules to the ductus epididymidis.
Most seminiferous tubules are in the form of loops, both ends of which join the rete testis by structures known as tubuli recti. These tubules are recognized by the gradual loss of spermatogenic cells, with an initial segment in which only Sertoli cells remain to form their walls, followed by a main segment consisting of cuboidal epithelium supported by a dense connective tissue sheath.
Tubuli recti empty into the rete testis, contained within the mediastinum, a thickening of the tunica albuginea. The rete testis is a highly anastomotic network of channels lined with cuboidal epithelium.
From the rete testis extend 10-20 ductuli efferentes. They have an epithelium composed of groups of nonciliated cuboidal cells alternating with ciliated cells that beat in the direction of the epididymis. This gives the epithelium a characteristic scalloped appearance. The nonciliated cells absorb much of the fluid secreted by the seminiferous tubules. The activity of ciliated cells and fluid absorption create a fluid flow that sweeps spermatozoa toward the epididymis. A thin layer of circularly oriented smooth muscle cells is seen outside the basal lamina of the epithelium. The ductuli efferentes gradually fuse to form the ductus epididymidis of the epididymis.
Excretory (extra testicular) Genital Ducts
Excretory genital ducts transport the spermatozoa produced in the testis toward the penile meatus. These ducts are the ductus epididymidis, the ductus (vas) deferens, and the urethra.

The
ductus epididymidis is a single highly coiled tube about 4-6 m in length. Together with surrounding connective tissue and blood vessels, this long canal forms the body and tail of the
epididymis. It is lined with pseudostratified columnar epithelium composed of rounded basal cells and columnar cells. These cells are supported on a basal lamina surrounded by smooth muscle cells, whose peristaltic contractions help to move the sperm along the duct, and by loose connective tissue rich in blood capillaries. Their surface is covered by long, branched, irregular microvilli called
stereocilia. The epithelium of the ductus epididymidis participates in the uptake and digestion of residual bodies that are eliminated during spermatogenesis.

From the epididymis the
ductus (
vas)
deferens, a straight tube with a thick, muscular wall, continues toward the prostatic urethra and empties into it. It is characterized by a narrow lumen and a mucosa with longitudinal folds, covered along most of its extent by pseudostratified columnar epithelium with stereocilia. The lamina propria is rich in elastic fibers, and the thick muscular layer consists of longitudinal inner and outer layers separated by a circular layer. The abundant smooth muscle produces strong peristaltic contractions that participate in the expulsion of the spermatozoa during ejaculation.

The ductus deferens forms part of the spermatic cord, which includes the testicular artery, the pampiniform plexus, and nerves. Before it enters the prostate, the ductus deferens dilates, forming a region called the
ampulla. In this area, the epithelium becomes thicker and extensively folded. At the final portion of the ampulla, the seminal vesicles join the duct. From there on, the ductus deferens enters the prostate, opening into the prostatic
urethra. The segment entering the prostate is called the
ejaculatory duct. The mucous layer of the ductus deferens continues through the ampulla into the ejaculatory duct, but the muscle layer ends after the ampulla.
MALE ACCESORY GENITAL GLANDS
The accessory genital glands produce secretions that are essential for the reproductive function in men. The accessory genital glands are the
seminal vesicles, the
prostate, and the
bulbourethral glands.
The Seminal Vesicles

The
seminal vesicles consist of two highly tortuous tubes about 15 cm in length. When the organ is sectioned, the same tube is observed in different orientations. It has a folded mucosa that is lined with cuboidal or pseudostratified columnar epithelium rich in secretory granules. These granules have ultrastructural characteristics similar to those found in protein-synthesizing cells. The lamina propria of the seminal vesicles is rich in elastic fibers and surrounded by a thin layer of smooth muscle. The seminal vesicles are not reservoirs for spermatozoa. They are glands that produce a viscid, yellowish secretion that contains spermatozoa-activating substances such as carbohydrates, citrate, inositol, prostaglandins, and several proteins. The carbohydrates, of which
fructose is the most abundant, are the source of energy for sperm motility. Seventy percent of human ejaculate originates in the seminal vesicles. The height of the epithelial cells of the seminal vesicles and the degree of activity of the secretory processes are dependent on testosterone levels.
The Prostate Gland

The prostate gland, the largest of the accessory glands, is pierced by the urethra and the ejaculatory ducts. The slender capsule of the gland is composed of a richly vascularized, dense irregular collagenous connective tissue interspersed with smooth muscle cells. The connective tissue stroma of the gland is derived from the capsule and is, therefore, also enriched by smooth muscle fibers in addition to their normal connective tissue cells.
The prostate gland, a conglomeration of 30 to 50 individual compound tubuloalveolar glands, is arranged in three discrete, concentric layers mucosal, submucosal, and main.
The mucosal glands are closest to the urethra and thus are the shortest of the glands. The submucosal glands are peripheral to the mucosal glands and are consequently larger than the mucosal glands. The largest and most numerous of the glands are the peripheralmost main glands, which compose the bulk of the prostate.
The lumina of the tubuloalveolar glands frequently house round to oval prostatic concretions (corpora amylacea), composed of calcified glycoproteins, whose numbers increase with a person’s age.
The prostatic secretion constitutes a part of semen. It is a serous, white fluid rich in lipids, proteolytic enzymes, acid phosphatase, fibrinolysin, and citric acid. The formation, synthesis, and release of the prostatic secretions are regulated by dihydrotestosterone, the active form of testosterone.
The Bulbourethral Glands

The
bulbourethral glands (
Cowper's glands), 3-5 mm in diameter, are proximal to the membranous portion of the urethra and empty into it. They are tubuloalveolar glands lined with mucus-secreting simple cuboidal epithelium. Skeletal and smooth muscle cells are present in the septa that divide each gland into lobes. The secreted mucus is clear and acts as a lubricant.
PENIS

The penis is composed of three columns of erectile tissue, each enclosed by its own dense, fibrous connective tissue capsule, the tunica albuginea.
Two of the columns of erectile tissue, the corpora cavernosa, are positioned dorsally; their tunicae albugineae are discontinuous in places, permitting communication between their erectile tissues. The third column of erectile tissue, the corpus spongiosum, is positioned ventrally. Because the corpus spongiosum houses the penile portion of the urethra, it is also called the corpus cavernosum urethrae. The corpus spongiosum ends distally in an enlarged, bulbous portion, the glans penis (head of the penis). The tip of the glans penis is pierced by the end of the urethra as a vertical slit.
The three corpora are surrounded by a common loose connective tissue sheath, but no hypodermis, and are covered by thin skin. Skin continues distal to the glans penis to form a retractable sheath, the prepuce. When an individual is circumcised, it is the prepuce that is removed.
Erectile tissue of the penis contains numerous variably shaped, endothelially lined spaces. The vascular spaces of the corpora cavernosa are larger centrally and smaller peripherally, near the tunica albuginea. However, the vascular spaces of the corpus spongiosum are similar in size throughout its extent.
Refferences :
- Gartner, L.P. and Hiatt, J.L. Concise Histology. 2011
- Color Textbook Histology, third edition, leslie P. Gartner
- Basic Histology, tenth edition, L. Carlos Junqueira,2003
- Histology and Cell Biology, second edition,2007
- Elsevier’s Integrated Histology,2007
 The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.
The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.

 Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.
Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.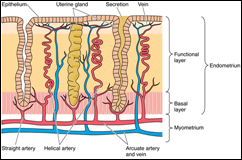 The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
















The Histology of Female Genital System Semester VI (2012)