Contents :
Female Reproductive System
Ovaries
Ovarian Follicles
Uterus
Menstrual Cycle
Mammary Gland
Female Reproductive System
 The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.
The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.
Ovaries
Ovarian Follicles

Primary Follicle

Secondary Follicle
 Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.
Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.
Uterus
 The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
Menstrual Cycle
Mammary Gland
Refferences :
Female Reproductive System
Ovaries
Ovarian Follicles
Uterus
Menstrual Cycle
Mammary Gland
Female Reproductive System
 The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.
The female reproductive system consists of the internal reproductive organs (the paired ovaries and oviducts, the uterus, and the vagina) and the external genitalia.
Although the mammary glands are not considered part of the female reproductive system, their physiology and function are so closely associated with the reproductive system.
The paired ovaries, located within the pelvis, are almond-shaped bodies 3 cm long, 1.5 to 2 cm wide, and 1 cm thick.
The surface epithelium covering the ovaries, called the germinal epithelium, is a modified peritoneum. Directly beneath this epithelium is the tunica albuginea, the connective tissue capsule whose collagen fibers are oriented parallel to the ovary surface.
Each ovary is subdivided into the highly cellular cortex and a medulla.
The ovarian cortex is composed of a connective tissue framework, the stroma, housing fibroblast-like stromal cells as well as ovarian follicles in various stages of development. The medulla contains large blood vessels, lymph vessels, and nerve fibers embedded in a connective tissue stroma.
Before the onset of puberty, all of the follicles of the ovarian cortex are in the primordial follicle stage. The pulsatile release of GnRH from the hypothalamus results in a similar, pulsatile, release of gonadotropins (follicle-stimulating hormone [FSH], and leutinizing hormone [LH]) from the basophils of the anterior pituitary that culminates in the commencement of follicular development and the onset of the ovulatory cycle.
The development of the primary follicles is independent of FSH; differentiation and proliferation of the follicular cells are triggered by local factors secreted by cells of the ovary. Secondary and later follicles, however, are under the influence of FSH. Follicular development usually culminates in the release of a single oocyte (ovulation).
Ovarian follicles are surrounded by stromal tissue and consist of a primary oocyte and its associated follicular cells arranged in a single spherical layer or several concentric layers around the primary oocyte.
There are four identifiable stages of follicular development based on the growth of the follicle and the development of the oocyte: Primordial follicles, unilaminar and multilaminar primary follicles, secondary (antral) follicles, and Graafian (mature) follicles.
The development of the primordial and primary follicles is independent of FSH; instead, the differentiation and proliferation of the follicular cells are triggered by as yet uncharacterized local factors secreted by cells of the ovary. Secondary and later follicles, however, are under the influence of FSH. Follicular development usually culminates in the release of a single oocyte (ovulation).
Primordial follicles, the most primitive follicles, are abundant before birth, after which they become fewer in number. The primordial follicle is composed of a primary oocyte, arrested in the prophase stage of meiosis I, is surrounded by a single layer of flattened follicular cells.

Primary Follicle

Primordial follicles develop into primary follicles distinguished as a result of changes in the primary oocyte, the follicular cells, and the surrounding stromal tissue.
The primary oocyte grows to about 100 to 150 μm in diameter with an enlarged nucleus (sometimes called the germinal vesicle).
Follicular cells become cuboidal in shape. As long as only a single layer of follicular cells encircles the oocyte, the follicle is called a unilaminar primary follicle. When the follicular cells proliferate and stratify, forming several layers of cells around the primary oocyte, the follicle is called a multilaminar primary follicle, and the follicular cells are more commonly referred to as granulosa cells.
During this stage, an amorphous substance (the zona pellucida) appears, separating the oocyte from the surrounding follicular cells. Microvilli of the oocyte and filopodia of the follicular cells invade the zonula pellucida and form gap junctions through which they communicate throughout follicular development.
Stromal cells form an inner theca interna, composed mostly of a richly vascularized cellular layer, and an outer theca externa, composed mostly of fibrous connective tissue. The theca interna cells produce the male sex hormone androstenedione, which enters the granulosa cells, where it is converted by the enzyme aromatase into the estrogen estradiol. The granulosa cells are separated from the theca interna by a thickened basal lamina.Secondary Follicle
 Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.
Secondary follicles are similar to primary follicles except for the presence of accumulations of liquor folliculi among the granulosa cells.
Continued proliferation of the granulosa cells of the secondary follicle depends on FSH released by basophil cells of the anterior pituitary.
As more fluid is produced, individual droplets of liquor folliculi coalesce to form a single, fluid-filled chamber, the antrum. The granulosa cells become rearranged so that the primary oocyte is now surrounded by a small group of granulosa cells that project out from the wall into the fluid-filled antrum. This structure is called the cumulus oophorus. The loosely arranged low cuboidal granulosa cells immediately adjacent to the zona pellucida move slightly away from the oocyte, but their filopodia remain within the zona pellucida, maintaining contact with the primary oocyte. This single layer of granulosa cells that immediately surrounds the primary oocyte is called the corona radiata.
Most of the follicles that reach this stage of development undergo atresia. A few secondary follicles continue to develop into mature follicles.
Graafian Follicles
Continued proliferation of the granulosa cells and continued formation of liquor folliculi result in the formation of a graafian (mature) follicle whose diameter reaches 2.5 cm by the time of ovulation. The graafian follicle may be observed as a transparent bulge on the surface of the ovary, nearly as large as the ovary itself.
The follicular cells of the wall of the follicle compose the membrana granulosa. Continued formation of liquor folliculi causes the cumulus oophorus composed of the primary oocyte, the corona radiata, and associated follicular cells to become detached from its base to float freely within the liquor folliculi.
By the 14th day of the menstrual cycle, estrogen produced mostly by the developing graafian follicle, but also by secondary follicles, causes elevation of blood estrogen to levels high enough to have the numerous effects, including the shutting off of FSH release and a surge in LH release.
The high blood levels of LH causes the completion of the first phase of meiosis I, resulting in the formation of the secondary oocyte. The secondary oocyte begins, and is arrested in, the metaphase stage of meiosis II. and is released from the graafian follice, a process known as ovulation.
The remnants of the graafian follicle are converted into the corpus hemorrhagicum and then the corpus luteum.
 The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
The uterus, a single, thick, pear-shaped structure located in the midline of the pelvis, receives at its broad, closed end the terminals of the paired oviducts. It is divided into three regions, the body, fundus, and the cervix.
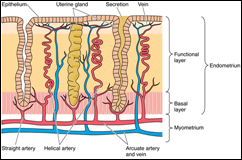
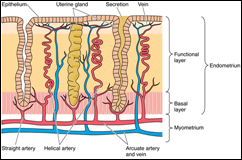
The uterine wall of the body and the fundus is composed of an endometrium, myometrium, and either an adventitia or a serosa.
The endometrium, or mucosal lining of the uterus, is composed of a simple columnar epithelium and a lamina propria. The epithelium is composed of nonciliated secretory columnar cells and ciliated cells, whereas the lamina propria houses simple branched tubular glands that extend as far as the myometrium The morphological and physiological alterations that occur in the endometrium during the phases of the menstrual cycle are controlled by various hormones.
The endometrium consists of two layers, the functionalis, a thick, superficial layer that is sloughed at menstruation and the basalis, a deep, narrow layer whose glands and connective tissue elements proliferate and thereby regenerate the functionalis during each menstrual cycle.
The functionalis is vascularized by numerous coiled helical arteries that supply the glands and connective tissue. The straight arteries are much shorter and supply only the basalis.
The myometrium is composed of inner longitudinal, middle circular, and outer longitudinal layers of smooth muscle.
Much of the anterior portion of the uterus is covered by adventitia , whereas the fundus and posterior portion of the body are covered by a serosa.
Menstruation, which begins on the day bleeding from the uterus starts, occurs when fertilization does not take place. The corpus luteum becomes nonfunctional about 14 days after ovulation, thus reducing the levels of progesterone and estrogen. Although the entire functionalis layer of the endometrium is sloughed, it is not completely released from the wall immediately; rather, this process continues for 3 to 4 days.
The proliferative phase (or follicular phase) occurs at the same time as the development of the ovarian follicles. It begins when the menstrual flow ceases, on about day 4, and continues through day 14 by which time the functionalis layer of the endometrium has been fully restored to its previous status with a full complement of epithelium, glands, stroma, and coiled arteries.
The secretory phase (or luteal phase) commences after ovulation. During this phase, the endometrium continues to thicken. The secretory products first accumulate in the basal region of the cytoplasm of the cells constituting the endometrial glands, the granules move apically, and are released into the lumen of the gland. This glycogen-rich material will nourish the conceptus before the formation of the placenta. The secretory phase completes the menstrual cycle as the 28th day approaches, presaging the menstrual phase of a new menstrual cycle.
Observe the correlation with the events occurring in the ovary as well as with the blood hormonal levels.
Mammary Gland
Mammary glands secrete milk, a fluid containing proteins, lipids, and lactose as well as lymphocytes and monocytes, antibodies, minerals, and fat-soluble vitamins.
The glands within the breasts are compound tubuloalveolar glands, consisting of 15 to 20 lobes radiating out from the nipple. Each lobe is drained by its own lactiferous duct where each duct is dilated to form a lactiferous sinus for milk storage and then narrows before reaching the nipple.
Resting or nonsecreting mammary glands of nonpregnant women have the same basic architecture as the lactating (active) mammary gland, except that they are smaller and without developed alveoli, which occur only during pregnancy.
Mammary glands are activated by elevated surges of estrogen and progesterone during pregnancy to become lactating glands to provide milk for the newborn. At this time, the terminal portions of the ducts branch and grow and the alveoli develop and mature
As pregnancy progresses, the breasts enlarge as a result of hypertrophy of the glandular parenchyma and engorgement with colostrum, a protein-rich fluid, in preparation for the newborn. Within a few days after birth, when estrogen and progesterone secretions have subsided, prolactin, secreted by acidophils of the anterior pituitary gland, activates the secretion of milk, which replaces the colostrum.
The secretions of the alveolar cells are of two kinds: lipids and proteins. Lipids are stored as droplets within the cytoplasm. They are released from the secretory cells, possibly by the apocrine mode of exocytosis. Proteins synthesized within these secretory cells are liberated from the cells by the merocrine mode of exocytosis.
- Color Textbook Histology, third edition, leslie P. Gartner
- Basic Histology, tenth edition, L. Carlos Junqueira,2003
- Histology and Cell Biology, second edition,2007
- Elsevier’s Integrated Histology,2007





The Histology of Female Genital System Semester VI (2012)